Heart failure – a global public health problem
Heart failure (HF) affects more than six million individuals in the US and nearly 100 million worldwide, causing poor quality of life, recurrent hospitalizations, and a high risk of death (1). HF is a progressive cardiac syndrome, and it impairs ventricles’ ability to fill with or eject blood. The most common and serious form is HF with reduced ejection fraction (HFrEF), where contractility is reduced, leading to impaired delivery of blood and oxygen to organs and tissues.
HF prevalence overall increases as individuals age, occurring in over 10-20% of those over 80 years (2). This may be attributed in part to increased survival in older patients after CV events like myocardial infarction.
HF is a leading cause of hospitalization, with over 50% of patients re-hospitalized within 6 months of discharge (3). Quality of life is significantly reduced, with advanced HF patients often requiring cardiac devices and/or surgical interventions. While mortality in HF is estimated at 60% within 5 years (4), those with HFrEF experience even worse prognosis, with mortality increasing with lower ejection fraction.
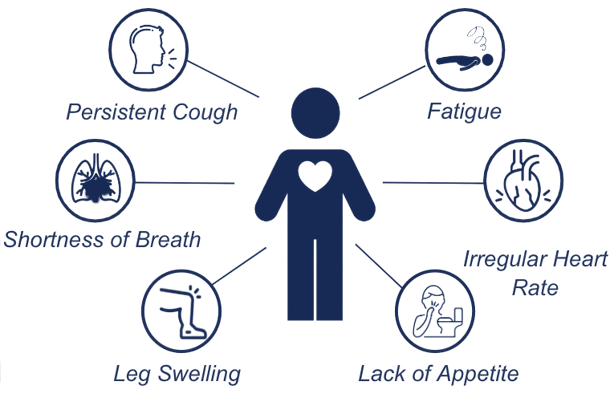
Symptoms limit daily activities and quality of life:
The foundational guideline-based medical therapy for HFrEF today consists of four different types of medications which all reduce the risk of HF hospitalization and death: ACEI/ARNI, beta-blockers, mineralocorticoid receptor antagonists, and SGLT2 inhibitors (5). Diuretics are used for symptom relief. In some patients, additional medications, devices and/or surgical interventions may be considered. However, patients with HFrEF still progress to advanced HF when contractility is severely impaired. In addition, the foundational drugs used may not be tolerated or effective. No current therapies safely target the underlying defect in heart failure: reduced contractility. Agents that do increase contractility, so called inotropes, are sometimes used in acute/advanced heart failure and may relieve symptoms, but they may cause life-threatening ventricular arrythmias, ischemia, hypotension and increase mortality. Thus, there is a clear unmet medical need for a “safe inotrope”.
”If you look at the therapeutic tools we have now, we have SGLT2s, we have Entresto, we have interventional devices, etc. but mortality at 1 year is still 20-50% in mild-moderate and over 50% in severe heart failure. It means that despite all the medications and interventions there is still unmet need for new drugs”
HFrEF Key Opinion Leader (KOL)
”Quadruplet therapies have overlapping side-effects so they tend to have an additive effect in some patients that results in discontinuation. If you were designing the perfect therapy, give me efficacy, but with no effects that further compound those from the rest of the quadruplet”
HFrEF High Volume Treater (HVT)
Feel free to contact us if you have any questions or want to book a meeting.
Contact us